Dying is hard, not just physically, but psychologically. It’s fraught with emotional landmines of worry for loved ones, traumas or regret over the past, and fear of the future. Hospice Austin social workers must delicately navigate these minefields in order to help patients achieve peace. It means building trust in often a short amount of time and entails helping patients and loved ones organize and process their feelings around mortality. Do you have your advance directives in place? Have you thought about whether you’d like to be buried or cremated? How do you feel about dying?
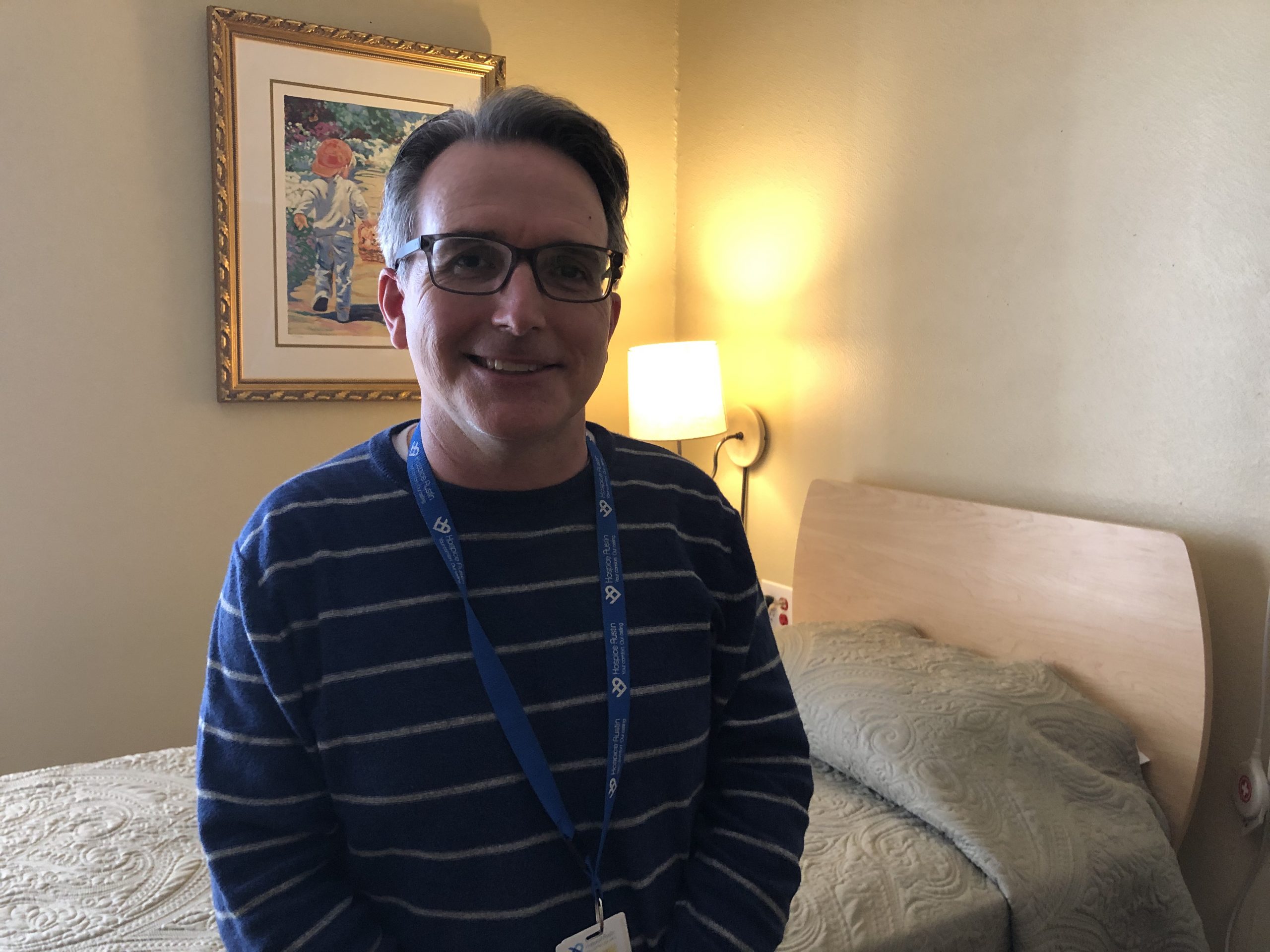
It’s important to delve deep enough to discover what the patient really wants. Hospice Austin’s Christopher House social worker Marc Sugars remembers a young man who came to Christopher House with a relatively treatable form of cancer. He was resigned to dying, estranged from his family who lived elsewhere, and had no money. After Marc and the rest of the Christopher House team started exploring his situation with him, they discovered that he discontinued his treatments because he couldn’t afford transportation. Within 4 days, they got him into a hospital for treatment. He’s now gone back to where his family lives and is continuing treatment and doing well.

Hospice Austin social worker Caroline Gonzales
Of course, the pandemic has made the job of social workers more challenging. Caroline Gonzales is a hospital-based social worker. Many of her patients are newly-diagnosed with a terminal illness, and some are unresponsive with just a few days left to live. Caroline’s job in those cases is caring for the loved ones. She’s had a lot of patients this year with COVID-19. Because visitation is limited, families feel disconnected. Caroline had a recent patient in his 40’s with the virus. He did not want to go on a ventilator under any circumstances and said he wanted to be on hospice care and let nature take its course. His parents didn’t understand what was going on. If he is on the BiPap, will he keep living?
“We discussed a lot of medical information and funeral planning. He was totally healthy and working before, and he had never had those discussions with them,” Caroline explained. “His parents visited for 15 minutes and he was unresponsive. It was really hard. I reassured them that he knows he’s loved and they have to do what helps them feel most at peace for themselves. His parents were able to pick out a funeral home and feel a little more settled.”
One of the most important aspects of a social worker’s role is to be an advocate for the patient. Some patients feel very mistrustful of medical professionals, so social workers try to elicit what’s most important to them and represent their interests wherever possible.

Hospice Austin social worker Amelia Frank
Amelia Frank works on the home team in a rural area. Many of her patients do not have financial resources and being sick can put a huge strain on families from loss of income both from the patient and the caregiver. Amelia spends a lot of her time problem-solving how families can take time off work, apply for county assistance or help through local churches, process anticipatory grief, complete advance directives, and make final arrangements.
Amelia said she gets a lot of satisfaction from her job when she takes the time to reflect on how a situation would have been different if the team hadn’t been involved. “We make a huge difference in these patients’ lives during a stressful time,” she said. “I had a patient who was formerly homeless. We had a really good relationship. A lot of [sick] people are very isolated and become depressed; even just their relationship with us improves their quality of life. We’re helping people solve problems, but sometimes just being able to make a good connection with them can be transformative.”